Prostate Cancer Diagnosis
Prostate cancer is one of the most common types of cancer among men. It typically develops in the prostate, a small gland located below the bladder and in front of the rectum. As with any type of cancer, early detection is crucial for effective treatment and improved outcomes. In this blog post, we will delve into the various aspects of prostate cancer diagnosis, including risk factors, symptoms, screening methods, and the role of modern technology in the early detection of this disease.
Understanding Prostate Cancer and Its Importance
Prostate cancer begins when abnormal cells in the prostate gland grow uncontrollably. While it is typically slow-growing, it can become aggressive and spread to other parts of the body if left untreated. One of the most significant factors in managing prostate cancer is early detection, which allows for treatment before the cancer spreads. Prostate cancer is particularly common in men over the age of 50, with a higher risk for those with a family history of the disease. It is essential to recognize the significance of prostate cancer diagnosis in saving lives and minimizing the impact of the disease on an individual’s health and quality of life.
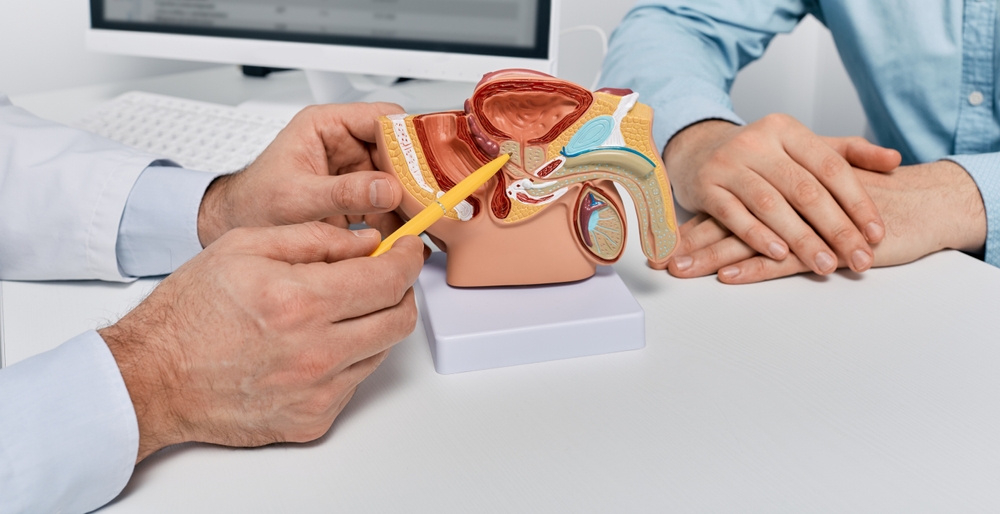
The prostate plays a key role in male reproductive health, producing seminal fluid that nourishes and transports sperm. As such, prostate cancer can disrupt not just physical well-being, but also sexual and urinary functions. The goal of a prostate cancer diagnosis is to detect the disease at an early stage, when it is most treatable, and to evaluate its progression to determine the best course of action for treatment.
Risk Factors for Prostate Cancer
Like many cancers, the risk of developing prostate cancer can be influenced by several factors, some of which are beyond an individual’s control. Age is one of the primary risk factors, with the likelihood of developing prostate cancer increasing significantly after the age of 50. African American men are also at higher risk, as they are more likely to develop aggressive forms of prostate cancer at a younger age. Genetics also play a significant role in determining prostate cancer risk. Men with a family history of prostate cancer, especially those with close relatives who have been diagnosed, are at greater risk of developing the disease themselves.
Diet and lifestyle choices may also contribute to the risk of prostate cancer, though the evidence is still being studied. High-fat diets, particularly those rich in red meats and processed foods, have been linked to an increased risk of prostate cancer. On the other hand, a diet rich in fruits, vegetables, and healthy fats may help reduce the risk. While these factors can influence prostate cancer risk, it is essential to note that many men who develop prostate cancer have no obvious risk factors. As such, routine screening and early diagnosis remain key elements in preventing the disease from advancing undetected.
Symptoms of Prostate Cancer
Prostate cancer often develops without causing any noticeable symptoms, particularly in its early stages. This is one of the reasons why regular screenings are important, even if a person feels healthy. As the cancer grows or if it begins to spread, however, some symptoms may emerge. The most common symptoms include frequent urination, especially at night, difficulty starting or stopping urination, weak or interrupted urine flow, and blood in the urine or semen. Men may also experience pain during urination or ejaculation, as well as persistent pain in the lower back, hips, or pelvis.
It is important to note that these symptoms can also be caused by conditions other than prostate cancer, such as benign prostatic hyperplasia (BPH) or prostatitis. BPH is a non-cancerous enlargement of the prostate, which can cause similar urinary symptoms. Therefore, the presence of these symptoms does not automatically indicate prostate cancer. It is essential to consult a healthcare provider if any of these symptoms are present so that further diagnostic tests can be conducted to determine the underlying cause.
Screening Methods for Prostate Cancer
Prostate cancer diagnosis typically begins with screening, especially for individuals at higher risk. There are two main screening methods for prostate cancer: the prostate-specific antigen (PSA) test and the digital rectal exam (DRE). The PSA test measures the level of prostate-specific antigen in the blood, a protein produced by the prostate gland. Elevated PSA levels can indicate the presence of prostate cancer, though other conditions like BPH or prostatitis can also cause a rise in PSA levels. For this reason, the PSA test alone is not conclusive, but it serves as an important first step in detecting prostate cancer.
The digital rectal exam (DRE) involves a physician inserting a gloved, lubricated finger into the rectum to feel the size, shape, and texture of the prostate. The exam can help detect abnormalities such as lumps, hardness, or irregularities in the prostate gland that may suggest cancer. While the DRE is a simple and quick procedure, it is not as effective as the PSA test for detecting prostate cancer, and it is typically used in conjunction with other diagnostic methods.
In some cases, if the PSA test or DRE results are abnormal, further testing may be required. A prostate biopsy, for example, involves taking small tissue samples from the prostate to check for cancer cells. This is the most definitive way to confirm a prostate cancer diagnosis. Imaging tests such as an ultrasound, MRI, or CT scan may also be used to help assess the size, location, and potential spread of the cancer.
The Role of Technology in Prostate Cancer Diagnosis
Advancements in medical technology have significantly improved the accuracy and effectiveness of prostate cancer diagnosis in recent years. One notable development is the use of multi-parametric MRI (mpMRI), which combines multiple imaging techniques to create detailed images of the prostate. mpMRI has become an invaluable tool for detecting prostate cancer, particularly in cases where the results of traditional tests like the PSA test and DRE are inconclusive. It can help identify suspicious areas in the prostate that may require a biopsy, allowing for a more targeted and precise diagnosis.
Another technological advancement is the use of genomic testing to better understand the genetic makeup of prostate cancer cells. Genomic tests can analyze the DNA of prostate cancer cells to determine how aggressive the cancer is likely to be. This information can help doctors make more informed decisions about treatment options, such as whether a patient may benefit from active surveillance, surgery, radiation therapy, or other interventions.
In addition, advances in artificial intelligence (AI) are helping to enhance the diagnostic process. AI algorithms can analyze medical images such as prostate biopsies and MRI scans, identifying patterns and abnormalities that might be missed by the human eye. This technology has the potential to greatly improve the accuracy of prostate cancer diagnosis, reduce the number of unnecessary biopsies, and help clinicians determine the best course of treatment for each individual.
Conclusion
Prostate cancer diagnosis plays a critical role in the early detection and treatment of this common yet serious disease. Regular screening, especially for those at higher risk, is essential for identifying prostate cancer before it progresses to more advanced stages. While symptoms can sometimes be a sign of the disease, early-stage prostate cancer is often asymptomatic, making routine screenings even more important. The use of advanced technologies, such as multi-parametric MRI and genomic testing, has revolutionized the way prostate cancer is diagnosed, allowing for more accurate assessments and better treatment decisions.
As our understanding of prostate cancer continues to evolve, it is essential for men to stay informed about the risk factors, symptoms, and screening methods available. By staying proactive and working closely with healthcare providers, individuals can increase their chances of detecting prostate cancer early and receiving timely, effective treatment. The continued development of diagnostic technologies and the focus on personalized medicine are expected to further improve the outcomes of prostate cancer diagnosis and treatment in the future.
 Rohit Kapoor, MD
Rohit Kapoor, MD